Episode 251: Combatting the Negative Effects of Sleep Deprivation
By listening to this episode, you can earn 1.25 Psychiatry CME Credits.
Other Places to listen: iTunes, Spotify
Article Authors: Brandon Luu, MD* David Puder, MD
The authors declare no conflicts of interest.
*Join Dr. Luu on X and on his substack.
Sleep is a fundamental biological necessity, intricately linked to nearly every system in the human body and should be the status symbol of choice in 2025. Yet, in our 24/7 society, voluntary and involuntary sleep restriction has become increasingly common, affecting both physical and cognitive performance. In healthy adults, these impairments can be rapid, profound, spanning from metabolic to cognitive disturbances.
Acute sleep deprivation is known to significantly impair cognitive performance. Studies have shown that after just 17-19 hours of continuous wakefulness, reaction times and attention levels deteriorate to a degree comparable to a blood alcohol concentration of 0.05%, while 24 hours without sleep can match or exceed the impairment seen at 0.10% BAC (Williamson & Feyer, 2000).
Memory is also greatly affected. For example, in one study, subjects were either sleep deprived for 36 hours or allowed to sleep normally prior to a learning session composed of sets of emotionally negative, positive, and neutral words. Participants who were sleep-deprived remembered ~40% less than those who had slept (Walker, 2008).
Note. Reprinted from “Sleep-dependent memory processing”, by Walker, M. P., 2008, Harvard Review of Psychiatry, 16(5), 287–298.
Chronic sleep deprivation also severely inhibits cognitive performance. After two weeks of restricting sleep to six hours per night, performance on psychomotor vigilance tests degrades to the level seen after one night of total sleep deprivation (Alhola & Polo-Kantola, 2007). The effect seems to be dose-dependent, with longer sleep deprivation leading to greater impairment.
Beyond these acute cognitive impairments, sleep deprivation also exerts widespread physiological consequences. Even one night of sleep loss can suppress natural killer cell activity by approximately 28% (Irwin et al., 1994), while two nights of four hours of sleep has been shown to decrease leptin by 18% and increase ghrelin by 28%, promoting increased hunger and caloric intake in healthy young men (Mosavat et al., 2021). Habitual short sleep is linked to elevated risk of obesity, type 2 diabetes, hypertension, and cardiovascular disease (Mullington et al., 2009). In one study of 11 healthy young men undergoing sleep restriction to just 4 hours per night for six nights, profound metabolic disturbances were observed. During this period, participants’ ability to regulate blood sugar dropped dramatically. It took 40% longer to clear glucose after a high-carb meal. Both insulin secretion and sensitivity fell by about 30%, changes that closely mimic the early stages of type 2 diabetes (Van Cauter et al., 2007).
Sleep also plays a critical role in brain health and emotional regulation. Functional MRI analysis has shown that after 35 hours of sleep deprivation, amygdala reactivity to negative stimuli increases by more than 60%. This suggests exaggerated emotional responses and poor impulse control (Yoo et al., 2007). In the long term, disrupted sleep may even increase risk of neurodegenerative processes. Chronic sleep deprivation has been associated with greater β-amyloid accumulation, impaired glymphatic clearance, and increased dementia risk (Garbarino et al., 2021).
Overall, sleep deprivation disrupts nearly every major biological system. It weakens immune defenses, elevates cardiovascular risk, impairs hormonal balance, and accelerates cognitive decline. Yet despite decades of compelling evidence, sleep remains undervalued in both medicine and public health. Additionally, for those who cannot avoid periods of sleep loss, it's essential to develop strategies that reduce its harm and support effective recovery.
Exercise vs. Sleep Deprivation
1. Saner et al., 2021: Protecting Metabolic Health
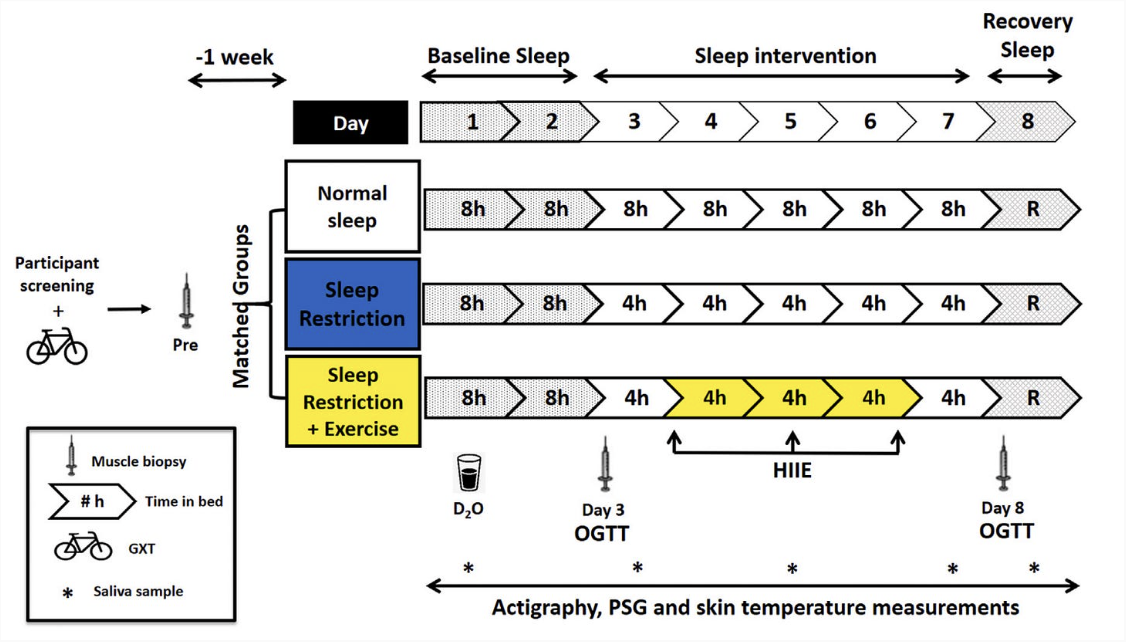
Note. Reprinted from “Exercise mitigates sleep-loss-induced changes in glucose tolerance, mitochondrial function, sarcoplasmic protein synthesis, and diurnal rhythms”, by Saner et al., 2021, Molecular metabolism, 43, 101110.
Methods: Participants restricted sleep to 4 hours per night for five consecutive nights. One group added three short high-intensity interval training (HIIT) sessions (10 intervals of 60 seconds at 90% peak power, 75 seconds rest).
Note. Reprinted from “Exercise mitigates sleep-loss-induced changes in glucose tolerance, mitochondrial function, sarcoplasmic protein synthesis, and diurnal rhythms”, by Saner et al., 2021, Molecular metabolism, 43, 101110.
Results: Without exercise, sleep restriction worsened glucose tolerance (+22% increase) and mitochondrial respiration (-18%). There was also reduced amplitude of diurnal rhythms, suggesting circadian rhythm dysfunction. The exercise group was protected from these metabolic impairments.
Mechanism: HIIT preserves mitochondrial respiratory capacity and enhances insulin-independent glucose uptake, which together help stabilise glucose tolerance and mitochondrial function during sleep loss.
TL;DR: Brief, intense HIIT sessions protect your metabolism from the negative effects of reduced sleep.
2. de Souza et al., 2017: Preventing Insulin Resistance
Methods: Eleven physically active men underwent 24 hours of total sleep deprivation after completing two weeks of HIIT (six sessions total, 8–12 intervals of 60 seconds at maximal effort with 75 seconds recovery).
Note. Reprinted from “High-Intensity Interval Training Attenuates Insulin Resistance Induced by Sleep Deprivation in Healthy Males”, by de Souza et al., 2017, Frontiers in physiology, 8, 992.
Results: Sleep deprivation alone significantly increased insulin resistance, glucose levels, and fatty acids. Two weeks of HIIT beforehand blunted these metabolic disturbances.
Note. Reprinted from “High-Intensity Interval Training Attenuates Insulin Resistance Induced by Sleep Deprivation in Healthy Males”, by de Souza et al., 2017, Frontiers in physiology, 8, 992.
Mechanism: Regular HIIT promotes insulin-independent glucose uptake (GLUT4 translocation) and boosts mitochondrial function, likely offsetting sleep-deprivation-induced insulin resistance.
TL;DR: Regular HIIT effectively "vaccinates" against insulin resistance caused by a single all-nighter.
3. Kojima et al., 2020 – Immediate Cognitive Boost
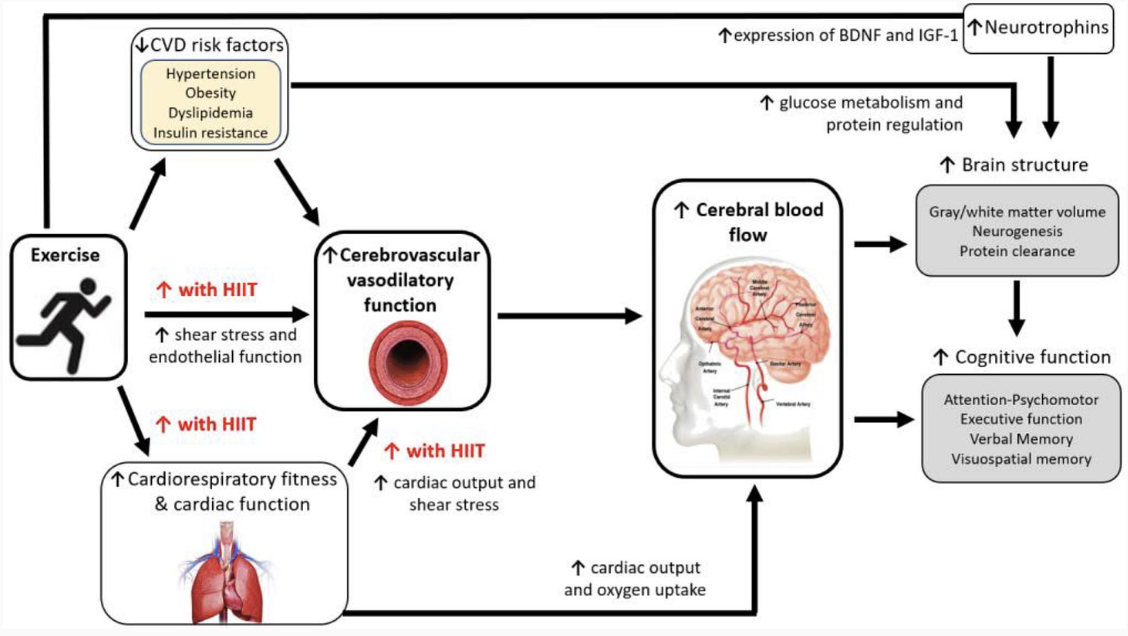
Sleep deprivation has been shown to decrease oxygen availability in the brain, so the thought is that improved cerebral blood flow from exercise could mitigate these effects.
Methods: University students underwent a challenge of 24 hours of sleep deprivation. They performed 20 minutes of moderate cycling (60% VO₂max) immediately afterward.
Results: Sleep deprivation impaired reaction time by about 14% and increased subjective fatigue. Exercise restored cognitive performance to about 7% less than the rested state while making the students feel less sleepy.
Mechanism: Moderate exercise increases brain circulation and arousal and activates neural circuits critical for attention and executive function.
Note. Reprinted from “Acute moderate-intensity exercise improves 24-h sleep deprivation-induced cognitive decline and cerebral oxygenation: A near-infrared spectroscopy study”, by Kojima et al., 2020. Respiratory physiology & neurobiology, 274, 103354.
TL;DR: A single 20-minute moderate cycling session quickly reverses cognitive impairment and fatigue after an all-nighter.
4. Williams et al., 2023: Handling Multiple Stressors
While the exact neurobiological mechanisms remain unclear, both sleep deprivation and hypoxia are thought to impair prefrontal cortex (PFC) function. This is a region critical for executive tasks like working memory, inhibition, and cognitive flexibility.
Methods: Participants faced sleep deprivation (three nights of four hours sleep or one night of total sleep deprivation) combined with acute hypoxia (low oxygen, similar to high altitude). They performed a single moderate-intensity cycling session (20 minutes at up to ~50% VO₂max).
Note. Reprinted from “The effects of sleep deprivation, acute hypoxia, and exercise on cognitive performance: A multi-experiment combined stressors study”, by Williams et al., 2024. Physiology & behavior, 274, 114409.
Results: The combination of total sleep deprivation and acute hypoxia significantly impaired cognitive performance. Oxygen saturation dropped and executive function was impaired by up to 30% in certain tasks.
Remarkably, a single 20-minute session of moderate cycling (~50% VO₂max) reversed the damage. 1-back and 3-back performance surpassed the rested baseline, improving by +5% and +25%, respectively. Choice reaction time improved by 24%, reducing the performance gap to just 12% below baseline.
Mechanism: Moderate exercise enhances cortical arousal and neuromodulator release, temporarily overriding cognitive deficits caused by sleep loss and hypoxia.
TL;DR: Even under combined severe stressors, brief moderate exercise restores cognitive function.
Creatine vs. Sleep Deprivation
1. Gordji-Nejad et al., 2024 – Single High Dose During Sleep Deprivation
A more recent study by Gordji-Nejad and colleagues examined whether a single, large dose of creatine could counteract the effects of partial sleep deprivation. Participants received a dose of 0.35 g/kg—roughly equivalent to 25–30 grams—just a few hours before undergoing a 21-hour period of sleep deprivation. Advanced magnetic resonance spectroscopy (MR spectroscopy) was used to assess changes in brain energy metabolites, including phosphocreatine (PCr) and ATP.
Key Findings:
Rapid Creatine Boost: The high-dose creatine led to a rapid increase in brain phosphocreatine, ATP, and other high-energy phosphate stores.
Enhanced Cognitive Performance: Participants who received creatine demonstrated better performance on tasks measuring cognitive speed and working memory. In some cases, their performance during sleep deprivation even surpassed their own baseline levels.
Time Course: The peak effect occurred approximately four hours after ingestion, with the benefits lasting for up to nine hours.
This study clearly indicates that even a single dose of creatine can rapidly reverse energy deficits in the brain, making it a valuable tool for acute situations such as unexpected overnight calls or jet lag.
Note. Reprinted from “Single dose creatine improves cognitive performance and induces changes in cerebral high energy phosphates during sleep deprivation”, by Gordji-Nejad et al., 2024. Scientific reports, 14(1), 4937.
2. McMorris et al., 2006 – 24 Hours of Sleep Deprivation
In a 2006 study by McMorris and colleagues, healthy adults were divided into two groups. One group received a high dose of creatine— 20 grams per day for seven days—while the other group received a placebo. After the supplementation period, both groups were kept awake for 24 hours under conditions of intermittent, mild exercise designed to standardize energy expenditure among participants. A comprehensive battery of cognitive tests was administered throughout the night to assess working memory, reaction time, and overall mood and fatigue.
Key Findings:
Reaction Time: Creatine users exhibited significantly less slowing of reaction time compared to the placebo group.
Executive Function: Participants in the creatine group performed better on tests of executive function, such as random movement generation at 24 hours of sleep deprivation.
Subjective Fatigue: Creatine-supplemented subjects reported less fatigue by the end of the 24-hour period.
This study was pivotal in demonstrating that creatine supplementation can preserve cognitive function during prolonged wakefulness, a finding that is highly relevant for those in high-stress, sleep-deprived situations.
Note. Reprinted from “Effect of creatine supplementation and sleep deprivation, with mild exercise, on cognitive and psychomotor performance, mood state, and plasma concentrations of catecholamines and cortisol”, by McMorris et al., 2006. Psychopharmacology, 185(1), 93–103.
3. Turner et al., 2015 – Hypoxia and Creatine
Turner and colleagues provided additional insight by investigating creatine’s effects under conditions of hypoxia—an environment in which oxygen levels are severely reduced, akin to high-altitude conditions. In this study, fifteen healthy adults supplemented with creatine (20 g/day for seven days) were exposed to 90 minutes of breathing air with only 10% oxygen.
Key Findings:
Cognitive Preservation: Under hypoxic conditions, cognitive scores for attention and executive function declined. However, in the creatine group, these cognitive measures were maintained at levels nearly comparable to normal conditions.
Neural Energy Metrics: The study found that creatine supplementation led to a significant increase in brain phosphocreatine levels (over 9%) and an increase in corticomotor excitability by 70%.
Implications: Despite severe oxygen deprivation, creatine helped sustain the brain’s energy reserves, thereby preserving cognitive function.
Turner et al.’s findings underscore the remarkable ability of creatine to support rapid ATP generation and neural energy production during times of acute stress, whether from sleep loss or low oxygen. This supports the concept that creatine acts as a crucial energy safety net for the brain under diverse stress conditions.
Note. Reprinted from “Creatine supplementation enhances corticomotor excitability and cognitive performance during oxygen deprivation”, by Turner et al., 2015. Journal of Neuroscience, 35(4), 1773–1780.
4. Kondo et al., 2016 – Dosing Strategies: 2 g vs. 4 g vs. 10 g
In a study focusing on adolescent females with treatment-resistant depression, Kondo and colleagues used advanced 31-phosphorus MR spectroscopy to measure brain phosphocreatine levels. Although the study population consisted of female teens on SSRI antidepressants, the findings are highly relevant for understanding creatine’s impact on brain energy metabolism under stress.
Study Design:
Participants were randomly assigned to receive either 2 g, 4 g, or 10 g of creatine daily for eight weeks, or a placebo.
The primary measurement was phosphocreatine (PCr) levels in the frontal lobe, assessed using 31P-MRS.
Depression scores were also monitored, though the focus here is on the energy metrics.
Key Findings:
The groups receiving 2 g and 4 g of creatine showed modest increases in brain PCr levels, approximately 4%.
In contrast, the group receiving 10 g daily exhibited a significantly greater increase in PCr, nearly double that of the lower-dose groups at about 9%.
Importantly, no major side effects or kidney issues were reported at the 10 g dose, addressing common safety concerns.
Interpretation: Kondo’s study provides evidence that a higher dose of creatine—around 10 g per day—may be optimal for saturating brain energy reserves. This finding challenges the conventional 3–5 g dose typically recommended for muscle performance and suggests that for cognitive resilience, higher dosing could be more beneficial.
Mechanism: How Creatine Supports the Sleep-Deprived Brain
Across several studies, a clear pattern emerges: creatine helps protect the brain under energy-depleting conditions.
Rapid ATP Resynthesis: Creatine donates phosphate groups to regenerate ATP, sustaining neuron function during metabolic stress.
Mitochondrial Stability: It improves mitochondrial function and reduces reactive oxygen species (ROS), especially under hypoxia.
Network Stability: It helps preserve frontoparietal network activity, essential for executive tasks and working memory.
Note. Reprinted from “Heads up” for creatine supplementation and its potential applications for brain health and function”, by Candow et al., 2023. Sports Medicine, 53 (Suppl 1), 49–65.
Caffeine
Effects of acute caffeine consumption following sleep loss on cognitive, physical, occupational and driving performance: A systematic review and meta-analysis (Irwin et al., 2019)
Methods: Systematic review and meta-analysis of 45 publications providing 327 effect estimates. Examined acute caffeine consumption on cognitive, physical, occupational and driving performance in sleep-deprived individuals. Average caffeine dose across studies was 340±170 mg.
Results:
Cognitive Performance:
Response time improved substantially (Hedges' g=0.86, 95% CI: 0.53-0.83).
Accuracy increased (g=0.68, 95% CI: 0.48-0.88).
Executive function improved moderately (g=0.35, 95% CI: 0.15-0.55).
Reaction time improved significantly (g=1.11, 95% CI: 0.75-1.47).
Information Processing:
Response time showed the largest improvement (g=1.95, 95% CI: 1.39-2.52).
Accuracy enhanced (g=0.43, 95% CI: 0.30-0.55).
Driving Performance:
Lateral vehicular control substantially improved (g=1.67, 95% CI: 1.32-2.02).
Longitudinal control improved (g=1.60, 95% CI: 1.16-2.03).
Dose-Response: Meta-regression revealed larger doses up to 600 mg provided greater benefits than lower doses.
Mechanism: Caffeine acts as an adenosine receptor antagonist, reducing neuronal inhibition and decreasing perceptions of effort during tasks.
TL;DR: Caffeine is highly effective at countering sleep loss impairments across attention, information processing, and driving safety, with larger doses (up to 600 mg) providing greater benefits, though research on dosage comparisons is limited.
Wesensten et al., 2002 – Modafinil vs. Caffeine Head-to-Head Comparison
Methods: Fifty healthy adults (37 men, 13 women; mean age 22.4 years) underwent 54-56 hours of total sleep deprivation. At 41.5 hours into sleep deprivation, participants received either placebo, modafinil (100 mg, 200 mg, or 400 mg), or caffeine (600 mg) in a double-blind design. Cognitive performance testing included psychomotor vigilance, reaction time tasks, mood assessments, and sleep latency measures.
Results:
Note. Reprinted from “Maintaining alertness and performance during sleep deprivation: Modafinil versus caffeine”, by Wesensten et al., 2002. Psychopharmacology (Berlin), 159(3), 238–247.
Sustained Attention (Psychomotor Vigilance Test):
Placebo PVT speed fell steadily throughout the night.
Modafinil 200 mg, 400 mg, and caffeine 600 mg maintained reaction speed at baseline from 02:00-11:00, preventing the performance decline seen with placebo.
Reaction Speed:
All groups showed performance dips at the circadian nadir (6:00 AM through 10:00 AM).
Both modafinil and caffeine mitigated these declines.
Subjective Sleepiness:
Compared with placebo, mean Stanford Sleepiness Scale (SSS) ratings were 30% lower with caffeine 600 mg, 24% lower with modafinil 400 mg, and 19% lower with modafinil 200 mg, indicating improved subjective alertness across all active treatments.
Ability to Stay Awake:
Sleep latency in a dark, supine test increased with modafinil 200/400 mg and caffeine 600 mg.
Side Effects:
Heart-pounding and nausea were reported more often with caffeine 600 mg and modafinil 400 mg.
Despite more frequent side effects, none were serious or debilitating.
Dose-Response:
Modafinil 100 mg was less effective than higher doses.
Both modafinil 200 mg and 400 mg produced comparable effects to caffeine 600 mg.
Performance effects were most notable during early morning hours (circadian trough).
Mechanism: Caffeine blocks adenosine receptors, removing neuronal inhibition, whereas modafinil inhibits dopamine and norepinephrine reuptake transporters. Despite different mechanisms, both drugs produced comparable performance restoration.
TL;DR: Modafinil 200-400 mg and caffeine 600 mg restore attention and vigilance during the critical early morning hours of extended sleep deprivation, though caffeine caused slightly more side effects and remains more practical due to availability and cost.
Bright Light Therapy
Comtet et al., 2019– Light therapy with boxes or glasses to counteract effects of acute sleep deprivation
Methods: Eighteen healthy young adults completed three separate 24-h total-sleep-deprivation nights, each ≥ 1 week apart.
Intervention at 05:00 (30 min):
10 000 lux white-light box (50 cm from eyes) [Dr. Puder recommends 1.5 feet away from you]
2 000 lux blue-enriched light glasses
Dim-light control < 8 lux
Results:
Sustained Attention (PVT)
At 7 A.M., the light therapy group had an almost 200ms improvement in PVT, a measure of attention.
Paced Visual Serial Addition Task (PVSAT)
Rapid-fire mental-arithmetic task that simultaneously taxes working memory, sustained attention, and processing speed. Drops in accuracy or speed provide a clear, quantitative read-out of cognitive fatigue.
Scores were preserved in the light therapy group but dropped about 25% at 7 A.M. in the control group.
Sleepiness
Significant improvement by about 1 point in the Karolinska Sleepiness Scale (KSS).
Note. Reprinted from “ Light therapy with boxes or glasses to counteract effects of acute sleep deprivation”, by Comtet et al., 2019. Scientific Reports, 9, 18073.
Mechanism: Bright light delivers an acute, non-circadian “alerting” signal. This is likely via melanopsin-rich retinal pathways plus rod/cone input to arousal centres, transiently overriding the rising sleep pressure during acute sleep deprivation. Because both broad-spectrum white (box) and blue-enriched (glasses) light worked, high illuminance rather than wavelength specificity appears sufficient.
TL;DR: 30-min of bright light at 05:00, whether from a 10 000-lux desk lamp or 2 000-lux wearable glasses, cuts subjective sleepiness and sharpens reaction time for the next two hours after an all-nighter.
Weisgerber et al., 2017--Driving home from the night shift: a bright light intervention study
Methods: Nineteen healthy adults (22.8 ± 4 years) completed three counterbalanced conditions separated by ≥1 week intervals. In the two sleep deprivation conditions, participants stayed awake overnight for 6 hours in dim light (35 lux), then received either 45 minutes of bright light (5600 lux) or continued dim light. They then completed a 44-minute simulated driving test (two laps) representing a commute home. In the rested condition, participants slept normally at home, received bright light upon waking, and completed the same driving test.
Results:
Crash Prevention:
26% of participants (5 out of 19) sustained a terminal accident (car flip) in the sleep deprivation + dim light condition.
Zero participants crashed in the sleep deprivation + bright light or rested conditions.
Performance Improvements:
Bright light reduced overall incidents and accidents compared to dim light during sleep deprivation.
Performance benefits were most evident on the second lap of the circuit (minutes 22-44 of the drive).
Effects appeared despite minimal changes in subjective sleepiness or reaction time.
Physiological Markers:
Bright light suppressed salivary melatonin as expected.
Oral temperature decreased and sleepiness increased across both sleep deprivation nights.
Bright light had little or no effect on subjective sleepiness ratings or psychomotor vigilance test reaction time.
Mechanism: Bright light delivers an acute alerting signal through melanopsin-rich retinal pathways to brain arousal centers, temporarily overriding rising sleep pressure. The alerting effect appears independent of circadian phase shifting and occurs without corresponding changes in subjective sleepiness perception.
TL;DR: 45 minutes of bright light exposure at the end of a night shift eliminated driving crashes and reduced accidents during a simulated morning commute, with safety benefits persisting throughout the drive despite participants not feeling substantially more alert.
Nicotine
Acute Nicotine Treatment Prevents REM Sleep Deprivation-Induced Learning and Memory Impairment in Rat (Aleisa et al., 2011)
Methods
Rats were assigned to: Control, Nicotine (1 mg/kg s.c. q12h), REM-sleep deprivation (24 h or 48 h), or Nicotine + REM-SD.
Cognitive testing: Radial-Arm Water Maze (assesses spatial learning and memory).
Results
Sleep deprived rats (48h) made significantly more errors compared to control. 4 mistakes vs. 0.45 mistakes on average.
Nicotine administration significantly improved the number of mistakes back to baseline (less than 1 mistake).
Flavanol-rich chocolate acutely improves arterial function and working memory performance counteracting the effects of sleep deprivation in healthy individuals Grassi et al., 2016
Methods: Thirty-two healthy participants completed four testing sessions: two baseline sessions after normal sleep and two experimental sessions after one night of total sleep deprivation. Two hours before each testing session, participants randomly consumed either high-flavanol chocolate bars or flavanol-poor chocolate bars. Testing included the Psychomotor Vigilance Task, a working memory task, office systolic blood pressure (SBP) and diastolic blood pressure (DBP), flow-mediated dilation (FMD), and pulse-wave velocity (PWV).
Results: Flavanol-rich chocolate preserved working memory performance in women after sleep deprivation, while having no significant effect on psychomotor vigilance. Sleep deprivation increased both SBP and DBP as well as PWV; however, these improved after flavonol-rich chocolate. Sleep deprivation impaired flow-mediated dilation, and flavanol-rich chocolate completely counteracted this vascular impairment.
Mechanism: Flavanol-rich chocolate acts through multiple pathways. Flavonoids induce nitric oxide-dependent vasodilation, which relaxes endothelial smooth muscle tone, counteracting vasoconstrictive effects of sleep deprivation. By enhancing blood cerebral blood flow, it supports higher-order cognitive functions.
TL;DR: A single dose of flavanol-rich dark chocolate two hours before tasks reverses the negative cardiovascular changes from sleep deprivation and preserves working memory performance, particularly in women.
The beneficial effects of green tea on sleep deprivation-induced cognitive deficits in rats: The involvement of hippocampal antioxidant defense Forouzanfar et al., 2021
Methods: Male rats were treated with saline, green tea extract (GTE) at 100 or 200 mg/kg/day, or epigallocatechin-3-gallate (EGCG) at 50 mg/kg/day intraperitoneally for 21 days. Animals were then trained in Morris water maze in a single day. Immediately after training, rats underwent 6 hours of total sleep deprivation via the gentle handling method, and were evaluated for spatial memory.
Results: Total sleep deprivation significantly impaired spatial memory, as shown by decreased time and distance spent in the target quadrant. Treatment with GTE at 200 mg/kg/day and EGCG at 50 mg/kg/day completely reversed these memory impairments to baseline levels. Thiol levels were significantly decreased with sleep deprivation and normalized with EGCG.
Mechanism: Green tea polyphenols, particularly EGCG, prevent memory deficits likely by normalizing the antioxidant hippocampal thiol defense system. Thiol groups eliminate reactive oxygen species through enzymatic and non-enzymatic pathways. During sleep deprivation, impaired antioxidant defenses (reduced thiol levels) contribute to memory impairment. With ECGC administration, thiol levels returned to baseline levels.
TL;DR: Three weeks of green tea extract (200 mg/kg/day) or EGCG (50 mg/kg/day) completely prevents memory impairment from 6-hour sleep deprivation by restoring antioxidant defenses in the hippocampus in mice.
Join Dr. Luu on X and on his substack.
References:
Aleisa, A. M., Helal, G., Alhaider, I. A., Alzoubi, K. H., Srivareerat, M., Tran, T. T., Al-Rejaie, S. S., & Alkadhi, K. A. (2011). Acute nicotine treatment prevents REM sleep deprivation-induced learning and memory impairment in rat. Hippocampus, 21(8), 899–909. https://doi.org/10.1002/hipo.20806
Alhola, P., & Polo-Kantola, P. (2007). Sleep deprivation: Impact on cognitive performance. Neuropsychiatric Disease and Treatment, 3(5), 553–567. https://doi.org/10.2147/ndt.s1216
Candow, D. G., Forbes, S. C., Ostojic, S. M., Prokopidis, K., Stock, M. S., Harmon, K. K., & Faulkner, P. (2023). “Heads up” for creatine supplementation and its potential applications for brain health and function. Sports Medicine, 53(Suppl 1), 49–65. https://doi.org/10.1007/s40279-023-01870-9
Comtet, H., Geoffroy, P. A., Kobayashi Frisk, M., Hubbard, J., Robin‑Choteau, L., Calvel, L., Hugueny, L., Viola, A. U., & Bourgin, P. (2019). Light therapy with boxes or glasses to counteract effects of acute sleep deprivation. Scientific Reports, 9, 18073. https://doi.org/10.1038/s41598-019-54311-x
de Souza, J. F. T., Dáttilo, M., de Mello, M. T., Tufik, S., & Antunes, H. K. M. (2017). High-Intensity Interval Training Attenuates Insulin Resistance Induced by Sleep Deprivation in Healthy Males. Frontiers in physiology, 8, 992. https://doi.org/10.3389/fphys.2017.00992
Forouzanfar, F., Gholami, J., Foroughnia, M., Payvar, B., Nemati, S., Khodadadegan, M. A., Saheb, M., & Hajali, V. (2021). The beneficial effects of green tea on sleep deprivation-induced cognitive deficits in rats: The involvement of hippocampal antioxidant defense. Heliyon, 7(11), Article e08336. https://doi.org/10.1016/j.heliyon.2021.e08336
Garbarino, S., Lanteri, P., Bragazzi, N. L., Magnavita, N., & Scoditti, E. (2021). Role of sleep deprivation in immune-related disease risk and outcomes. Communications Biology, 4(1), 1304. https://doi.org/10.1038/s42003-021-02825-4
Gordji-Nejad, A., Matusch, A., Kleedörfer, S., Jayeshkumar Patel, H., Drzezga, A., Elmenhorst, D., Binkofski, F., & Bauer, A. (2024). Single dose creatine improves cognitive performance and induces changes in cerebral high energy phosphates during sleep deprivation. Scientific reports, 14(1), 4937. https://doi.org/10.1038/s41598-024-54249-9
Grassi, D., Socci, V., Tempesta, D., Ferri, C., De Gennaro, L., Desideri, G., & Ferrara, M. (2016). Flavanol-rich chocolate acutely improves arterial function and working memory performance counteracting the effects of sleep deprivation in healthy individuals. Journal of hypertension, 34(7), 1298–1308. https://doi.org/10.1097/HJH.0000000000000926
Irwin, M. R., Mascovich, A., Gillin, J. C., Willoughby, R. A., Pike, J. L., & Smith, T. L. (1994). Partial sleep deprivation reduces natural killer cell activity in humans. Psychosomatic Medicine, 56(6), 493–498. https://doi.org/10.1097/00006842-199411000-00004
Irwin, C., Khalesi, S., Desbrow, B., & McCartney, D. (2019). Effects of acute caffeine consumption following sleep loss on cognitive, physical, occupational and driving performance: A systematic review and meta-analysis. Neuroscience & Biobehavioral Reviews, 102, 1–17. https://doi.org/10.1016/j.neubiorev.2019.12.008
Kojima, S., Abe, T., Morishita, S., Inagaki, Y., Qin, W., Hotta, K., & Tsubaki, A. (2020). Acute moderate-intensity exercise improves 24-h sleep deprivation-induced cognitive decline and cerebral oxygenation: A near-infrared spectroscopy study. Respiratory physiology & neurobiology, 274, 103354. https://doi.org/10.1016/j.resp.2019.103354
Kondo, D. G., Forrest, L. N., Shi, X., Sung, Y.-H., Hellem, T. L., Huber, R. S., & Renshaw, P. F. (2016). Creatine target engagement with brain bioenergetics: A dose-ranging phosphorus-31 magnetic resonance spectroscopy study of adolescent females with SSRI-resistant depression. Amino Acids, 48(8), 1941–1954. https://doi.org/10.1007/s00726-016-2194-3
McMorris, T., Harris, R. C., Swain, J., Corbett, J., Collard, K., Dyson, R. J., Dye, L., Hodgson, C., & Draper, N. (2006). Effect of creatine supplementation and sleep deprivation, with mild exercise, on cognitive and psychomotor performance, mood state, and plasma concentrations of catecholamines and cortisol. Psychopharmacology, 185(1), 93–103. https://doi.org/10.1007/s00213-005-0269-z
Mosavat, M., Mirsanjari, M., Arabiat, D. H., Smyth, A., & Whitehead, L. (2021). The role of sleep curtailment on leptin levels in obesity and diabetes mellitus. Obesity Facts, 14(2), 214–221. https://doi.org/10.1159/000514095
Mullington, J., Haack, M., Tóth, M., Serrador, J. M., & Meier-Ewert, H. K. (2009). Cardiovascular, inflammatory, and metabolic consequences of sleep deprivation. Progress in Cardiovascular Diseases, 51(4), 294–302. https://doi.org/10.1016/j.pcad.2008.10.003
Saner, N. J., Lee, M. J., Kuang, J., Pitchford, N. W., Roach, G. D., Garnham, A., Genders, A. J., Stokes, T., Schroder, E. A., Huo, Z., Esser, K. A., Phillips, S. M., Bishop, D. J., & Bartlett, J. D. (2021). Exercise mitigates sleep-loss-induced changes in glucose tolerance, mitochondrial function, sarcoplasmic protein synthesis, and diurnal rhythms. Molecular metabolism, 43, 101110. https://doi.org/10.1016/j.molmet.2020.101110
Turner, C. E., Byblow, W. D., & Gant, N. (2015). Creatine supplementation enhances corticomotor excitability and cognitive performance during oxygen deprivation. Journal of Neuroscience, 35(4), 1773–1780. https://doi.org/10.1523/JNEUROSCI.3113-14.2015
Van Cauter, E., Holmbäck, U., & Knutson, K. L. (2007). Impact of sleep and sleep loss on neuroendocrine and metabolic function. Hormone Research in Paediatrics, 67(1), 2–9. https://doi.org/10.1159/000097543
Walker, M. P. (2008). Sleep-dependent memory processing. Harvard Review of Psychiatry, 16(5), 287–298. https://doi.org/10.1080/10673220802432517
Weisgerber, D. M., Nikol, M., & Mistlberger, R. E. (2017). Driving home from the night shift: A bright light intervention study. Sleep Medicine, 30, 171–179. https://doi.org/10.1016/j.sleep.2016.09.010
Wesensten, N. J., Belenky, G., Kautz, M. A., Thorne, D. R., Reichardt, R. M., & Balkin, T. J. (2002). Maintaining alertness and performance during sleep deprivation: Modafinil versus caffeine. Psychopharmacology (Berlin), 159(3), 238–247. https://doi.org/10.1007/s002130100916
Williams, T. B., Badariotti, J. I., Corbett, J., Miller-Dicks, M., Neupert, E., McMorris, T., Ando, S., Parker, M. O., Thelwell, R. C., Causer, A. J., Young, J. S., Mayes, H. S., White, D. K., de Carvalho, F. A., Tipton, M. J., & Costello, J. T. (2024). The effects of sleep deprivation, acute hypoxia, and exercise on cognitive performance: A multi-experiment combined stressors study. Physiology & behavior, 274, 114409. https://doi.org/10.1016/j.physbeh.2023.114409
Williamson, A., & Feyer, A.-M. (2000). Moderate sleep deprivation produces impairments in cognitive and motor performance equivalent to legally prescribed levels of alcohol intoxication. Occupational and Environmental Medicine, 57(10), 649–655. https://doi.org/10.1136/oem.57.10.649
Yoo, S.-S., Gujar, N., Hu, P., Jolesz, F. A., & Walker, M. P. (2007). The human emotional brain without sleep: A prefrontal–amygdala disconnect. Current Biology, 17(20), R877–R878. https://doi.org/10.1016/j.cub.2007.08.007